The act of administering a medication via injection is one of the most fundamental and versatile procedures in modern pharmacology, yet the efficacy and safety profile of that single act are overwhelmingly dictated by its route of administration. When a substance is introduced directly into the body using a needle and syringe, the primary distinction that governs its entire pharmacological journey is whether the delivery is local (focal) or systemic (generalized). This is not merely a geographic difference; it represents two entirely separate therapeutic philosophies, each with its own advantages, inherent limitations, and clinical objectives. A local injection seeks to achieve a maximal concentration of the drug at the precise site of pathology, minimizing its spread and subsequent effect on non-diseased tissue. Conversely, a systemic injection utilizes the body’s highly efficient circulatory network—the bloodstream—as a transport mechanism, aiming for a consistent, therapeutic concentration throughout the entire body to treat a generalized or diffuse condition. The choice between these two modalities fundamentally influences everything from the required drug dosage and the onset of action to the pattern of potential side effects and the overall patient outcome. Understanding this physiological divergence is paramount for both prescribing clinicians and informed patients navigating complex treatment regimens.
The Choice Between These Two Modalities Fundamentally Influences Everything From the Required Drug Dosage and the Onset of Action to the Pattern of Potential Side Effects
The choice between these two modalities fundamentally influences everything
A local injection is, by design, an act of precision and immediate targeting. The core objective is to deliver the therapeutic agent directly into the micro-environment of the diseased tissue, maximizing the therapeutic index at the pathology site while maintaining the lowest possible systemic exposure. This focal delivery minimizes the likelihood of off-target effects in remote organs. Common examples include an intra-articular injection of corticosteroids into a knee joint to treat localized arthritis-related inflammation, or the injection of a local anesthetic directly into the tissue surrounding a surgical site to block nerve signals for immediate pain relief. In these instances, the clinician is consciously bypassing the complex, time-consuming process of absorption, distribution, and first-pass metabolism that a drug would endure if taken orally. The immediate physical presence of the medication where it is needed translates into a rapid onset of action and often allows for the use of a significantly lower total dose of the drug compared to what would be necessary if the drug had to saturate the entire circulatory system to reach the target site.
The Core Objective Is to Deliver the Therapeutic Agent Directly Into the Micro-Environment of the Diseased Tissue, Maximizing the Therapeutic Index at the Pathology Site
The core objective is to deliver the therapeutic agent directly into the micro-environment
The challenge with the local approach often revolves around ensuring the medication remains at the target site for the necessary duration without excessively diffusing away, a phenomenon termed drug clearance. The effectiveness of a local injection is intrinsically linked to the anatomical microvasculature of the injection site. Highly vascular areas, such as muscle tissue, will rapidly absorb and clear the drug into the systemic circulation, potentially limiting the duration of the local therapeutic effect, which is why a corticosteroid is often paired with a less soluble depot preparation when injected into a joint capsule. Conversely, poorly vascularized tissues, such as the cartilage within a joint, may hold the medication longer, providing sustained focal benefit. The successful delivery and retention of the drug depend heavily on the accuracy of the injection technique, often requiring image guidance (such as fluoroscopy or ultrasound) to confirm precise needle placement and avoid collateral damage to adjacent structures, particularly nerves or blood vessels.
The Effectiveness of a Local Injection Is Intrinsically Linked to the Anatomical Microvasculature of the Injection Site
The effectiveness of a local injection is intrinsically linked to the anatomical microvasculature
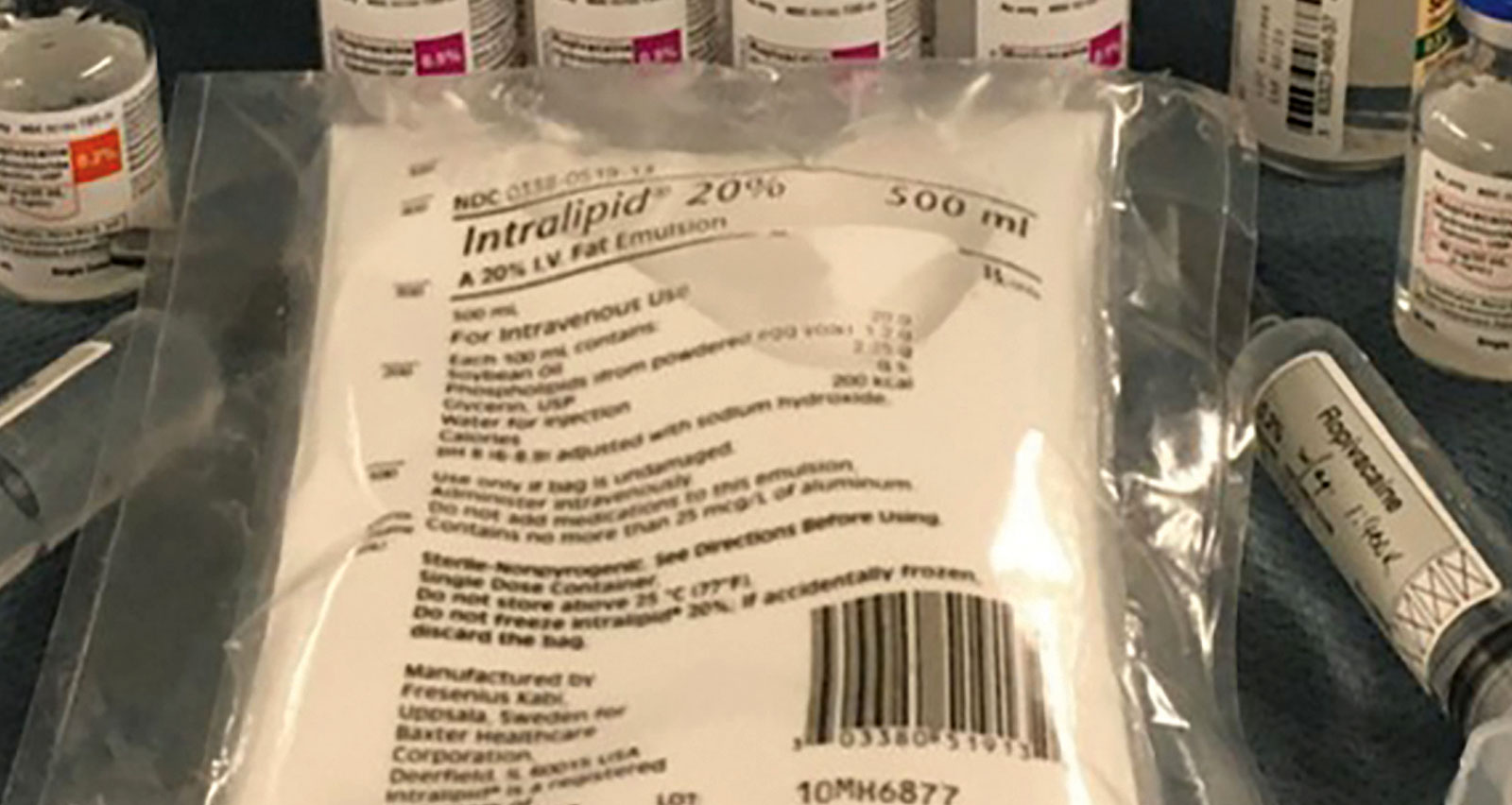
In stark contrast to the focal precision of local delivery, systemic injections are designed for diffuse action, utilizing the entire body’s volume to achieve a therapeutic drug level everywhere simultaneously. The fundamental purpose here is to treat conditions that affect multiple organs or are widespread throughout the entire organism, such as a severe bacterial infection (intravenous antibiotics) or a systemic inflammatory disorder (intramuscular methotrexate). The primary routes for systemic administration are intravenous (IV), intramuscular (IM), and subcutaneous (SC). The IV route is the most immediate, delivering the drug directly into the bloodstream with 100% bioavailability, leading to an instantaneous therapeutic effect, which is essential in emergency situations. IM and SC injections rely on absorption from the tissue into the bloodstream, a slower process that provides a more sustained, protracted release of the medication over a period of hours or even days, which is often preferable for vaccines or long-acting hormonal therapies.
The Primary Routes for Systemic Administration Are Intravenous (IV), Intramuscular (IM), and Subcutaneous (SC)
The primary routes for systemic administration are intravenous (IV), intramuscular (IM), and subcutaneous (SC)
The pharmacokinetic profile of a drug delivered systemically is dictated by a cascade of physiological events: Absorption, Distribution, Metabolism, and Excretion (ADME). Unlike local delivery, where metabolism and distribution are minor factors, a systemically administered drug must navigate the body’s highly complex biochemical processing pathways. The drug is first distributed throughout the circulatory system and body tissues, often binding to plasma proteins. It is then subjected to metabolism, primarily in the liver (a key site of drug modification), where it can be converted into active or inactive metabolites. Finally, the drug and its metabolites are excreted, typically via the kidneys or bile. The half-life of a systemically administered drug—the time it takes for its concentration in the blood to reduce by half—is a critical factor in determining the required dosing frequency and is entirely dependent on the efficiency of this ADME process, ensuring that the blood concentration remains within the narrow therapeutic window to be effective without becoming toxic.
The Half-Life of a Systemically Administered Drug—the Time It Takes for Its Concentration in the Blood to Reduce by Half—is a Critical Factor in Determining the Required Dosing Frequency
The half-life of a systemically administered drug—the time it takes for its concentration in the blood to reduce by half—is a critical factor
The inherent trade-off with systemic administration is the necessary acceptance of a higher risk of generalized side effects. Because the drug reaches all tissues, not just the target site, any organ possessing receptors or cellular machinery sensitive to the medication is potentially susceptible to its effects. For instance, an antibiotic administered systemically to combat an infection in the lungs will simultaneously pass through the gastrointestinal tract, potentially leading to widespread dysbiosis (disruption of the natural gut flora) and common side effects like diarrhea. Similarly, systemic chemotherapy agents, designed to kill rapidly dividing cancer cells, will also affect rapidly dividing healthy cells in the bone marrow and hair follicles, leading to the well-known toxicities of neutropenia and hair loss. This pervasive action, while necessary for widespread disease management, is the primary limiting factor in the tolerated dose and duration of systemic therapies, forcing clinicians to constantly balance therapeutic efficacy against patient tolerance and safety.
Because the Drug Reaches All Tissues, Not Just the Target Site, Any Organ Possessing Receptors or Cellular Machinery Sensitive to the Medication Is Potentially Susceptible to Its Effects
Because the drug reaches all tissues, not just the target site, any organ possessing receptors or cellular machinery sensitive to the medication is potentially susceptible
A fascinating area of convergence and clinical innovation involves the use of local delivery systems to achieve a prolonged systemic effect or, conversely, highly sophisticated systemic agents with focalized tissue affinity. Long-acting subcutaneous implants or intramuscular depot injections are examples of local delivery that serve a systemic purpose. Here, the drug is placed in a non-vascularized depot (e.g., in fat or muscle) designed to slowly dissolve or leak into the systemic circulation over weeks or months, ensuring consistent, low-dose systemic exposure without the need for daily dosing. On the other hand, cutting-edge pharmacological research is focused on creating targeted systemic therapies, such as liposomal drug delivery or antibody-drug conjugates (ADCs). These agents are administered systemically (via IV) but are specifically engineered to accumulate or become activated primarily at sites of pathology, such as tumor tissue, effectively achieving a localized therapeutic action while circulating through the entire body, bridging the gap between the two modalities.
These Agents Are Administered Systemically (via IV) But Are Specifically Engineered to Accumulate or Become Activated Primarily at Sites of Pathology, Such as Tumor Tissue
These agents are administered systemically (via IV) but are specifically engineered to accumulate or become activated primarily at sites of pathology
Considering the distinct risk-benefit profiles, the decision to use a local versus a systemic injection must be rooted in a precise differential diagnosis and a clear statement of therapeutic goals. If the pathology is discrete and contained (e.g., a single inflamed bursa or a neuroma), the localized approach is almost always preferable due to the potential for immediate, high-concentration efficacy and minimal systemic risk. If the disease is diffuse, metastatic, or generalized (e.g., rheumatoid arthritis affecting multiple joints, sepsis, or lymphoma), then systemic therapy is necessitated by the widespread nature of the pathology. The primary danger arises when a clinician attempts to treat a systemic disease with localized injections, which often leads to repeated injections, escalating local tissue damage, and still insufficient control over the generalized condition. Conversely, treating a purely localized issue with a high-dose systemic therapy unnecessarily exposes the entire body to potential toxicity.
If the Pathology Is Discrete and Contained (e.g., a Single Inflamed Bursa or a Neuroma), the Localized Approach Is Almost Always Preferable Due to the Potential for Immediate, High-Concentration Efficacy and Minimal Systemic Risk
If the pathology is discrete and contained (e.g., a single inflamed bursa or a neuroma), the localized approach is almost always preferable
Finally, the discussion of injection modality must account for patient compliance and preference, factors that significantly impact long-term therapeutic success. Systemic injections, particularly those delivered intramuscularly or subcutaneously, are often suitable for self-administration by the patient (e.g., insulin, heparin, certain fertility drugs), providing independence and flexibility in management. Local injections, however, almost invariably require the expertise and controlled setting of a clinical environment due to the precision and potential risks involved. For chronic conditions requiring frequent dosing, the convenience and reduced necessity of continuous clinical visits associated with a self-administered systemic schedule can significantly improve patient adherence and quality of life. Thus, while the biological mechanics define the possibility of a treatment, the patient’s ability and willingness to adhere to the prescribed delivery method often determine its practical success in the real world.
For Chronic Conditions Requiring Frequent Dosing, the Convenience and Reduced Necessity of Continuous Clinical Visits Associated With a Self-Administered Systemic Schedule Can Significantly Improve Patient Adherence
For chronic conditions requiring frequent dosing, the convenience and reduced necessity of continuous clinical visits
The division between local and systemic injection dictates whether medicine is a highly focused surgical strike against an isolated target or a necessary saturation campaign across the entire physiological landscape.
